Modern Drug Detection Techniques: Sampling Swab Drug Tests and Others
A high-profile case recently brought the importance of drug testing into the public eye. Embattled former TV host Andrew O'Keefe was charged after allegedly failing a random roadside drug test in Sydney's eastern suburbs. The incident highlights the critical role that sampling swab drug tests play in modern drug detection techniques, as well as the potential consequences for those who are caught using illicit substances.
In this article, we will examine the science behind sampling swab drug tests, their effectiveness in detecting drugs in drivers, and the broader implications for public safety and law enforcement. We will also discuss the challenges faced by authorities in combating drug-impaired driving and explore potential solutions to reduce the prevalence of this dangerous behavior.
Oral Fluid
In the last decade, a growing body of scientific literature has validated the use of oral fluid for drug testing, highlighting its effectiveness and reliability. Oral fluids typically contain the parent drug, although metabolites may also be present, offering additional insights. The higher concentration of parent drugs in oral fluids compared to drug metabolites further supports the use of this testing method.
Oral fluid specimens, compared to urine specimens, provide fewer opportunities for adulteration or substitution, which bolsters their credibility. Studies have shown that commercial adulterants or mouthwashes do not interfere with immunoassays, and they do not impact test results if used more than 30 minutes before specimen collection. However, it is important to note that the detection window for oral fluid is narrower than that of urine, and drug concentrations are generally lower. Oral fluid drug testing typically detects drug use within the previous 24-48 hours, regardless of the administration route. The selection of cutoffs also plays a crucial role in determining the detection window's length.
Various oral fluid collection devices exist, but the most common version consists of a swab or absorbent pad on a stick. This device is placed between the lower cheek and gums to collect fluid and left for a few minutes. Afterward, it is inserted into a vial containing a buffer solution and sent to the laboratory. Point-of-care tests (POCTs) are also available for oral fluid testing.
Sometimes, dry mouth syndrome can hinder oral fluid collection, necessitating several minutes to collect an adequate sample. Certain medications and illicit drugs may cause a dry mouth, and some oral fluid collection devices facilitate the process by stimulating oral fluid flow. Patients should avoid eating immediately before testing, as some foods may inhibit oral fluid production. If a patient's oral fluid contains blood, an alternative specimen, such as blood or urine, is required. The smaller sample size of oral fluid, compared to urine, limits the number of repeat or confirmatory tests that can be performed on the specimen.

Seeking steadfast, user-friendly saliva collectors to cater to your forensic endeavors? Behold, the marvel of Mantacc! Crafted to pinpoint the constituents of salivary samples, our kits are indispensable allies in forensic biology, toxicology, and drug surveillance. Mantacc's kits assure precise outcomes in your investigative quests, and their simplicity welcomes the dexterity of seasoned professionals and novices alike. Banish inferior collectors - embrace the excellence and dependability of Mantacc. Procure your saliva collection kits posthaste, and witness the distinction firsthand!
Sweat
A variety of collection devices have been developed for gathering sweat specimens, with the two most common being the patch and the swipe. However, only the sweat patch has received approval from the U.S. Food and Drug Administration (FDA). The amount of sweat collected depends on the duration of patch wear and the individual's physiology. To ensure sufficient sweat is collected for testing, the patch should be worn for a minimum of 3 days but no longer than 7 days. Most drugs will have been excreted within the first 48 hours, and this time frame allows for detecting drug use that occurred shortly before the patch was applied and throughout the device's time on the skin.
Before applying the patch, the skin should be thoroughly cleaned with soap and water, followed by swabbing with alcohol. A staff member, rather than the patient, must apply the patch to the skin. After 7 days, a practitioner removes the patch and sends it to the laboratory for analysis. Sweat samples primarily contain the parent drug, but some drug metabolites may also be detected. Drugs and drug metabolites identified in sweat include tetrahydrocannabinol (THC), amphetamine, methamphetamine, methylenedioxymethamphetamine (MDMA, or "Ecstasy"), codeine, morphine, heroin metabolite, phencyclidine (PCP), and cocaine and its metabolites (e.g., benzoylecgonine, ecgonine methyl ester).
Since sweat can only be collected in limited quantities, there might not be enough specimen for repeat or confirmatory testing. However, sweat is less susceptible to tampering or adulteration than urine. The accuracy of sweat testing is not standardized and remains somewhat controversial, calling for more research. Despite these concerns, the sweat patch is extensively used in the criminal justice system, and courts have upheld its use for identifying relapse or probation violations.

Blood
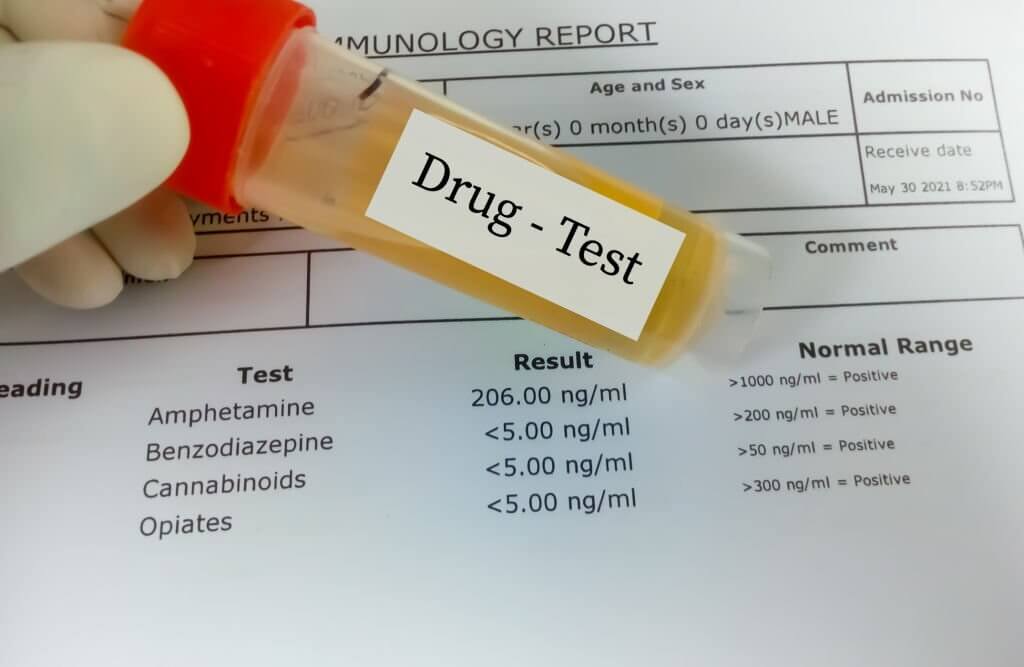
Blood testing is a valuable method for detecting alcohol or drug use, with its effectiveness beginning shortly after substance consumption, depending on the specific drug and administration route. In general, blood offers a shorter detection period compared to urine, making it suitable for detecting recent substance use. However, it is important to consider the procedural differences between blood and urine testing.
Blood collection is more invasive than other testing methods, such as urine or oral fluid collection, and demands trained personnel to obtain the specimen and conduct laboratory analysis. This requirement for skilled professionals may lead to logistical challenges in certain situations. Additionally, blood testing can be particularly problematic for individuals who inject drugs or those with poor venous access, as drawing blood may prove difficult in these cases.
Despite these challenges, blood testing remains a reliable option for identifying recent drug or alcohol consumption. Its accuracy and ability to detect a wide range of substances make it an essential tool in various settings, such as emergency rooms, drug treatment centers, and forensic investigations. Furthermore, blood testing can provide quantitative results that help determine the level of intoxication or impairment, which is particularly relevant in legal cases, such as driving under the influence (DUI) or workplace accidents.
Hair
The principle behind drug detection in hair is straightforward: drugs or their metabolites circulate in a person's bloodstream, and hair follicles absorb these substances from the bloodstream and from sebaceous and sweat gland secretions in the scalp. As the hair grows at a rate of about 1 cm per month, trace amounts of drugs become entrapped in the core of the hair. Consequently, drug metabolites can be detected in the hair shaft approximately 7-10 days after ingestion.
Hair analysis offers unique benefits, such as providing retrospective information on drug use, as opposed to the point-in-time information provided by urine, blood, and breath. However, some factors can disrupt hair testing's ability to determine historical use, such as drugs moving down the hair shaft via sweat or environmental drug exposure.
The hair sample, usually taken from the back of the head, can be collected from other body parts (e.g., face, armpit) for bald or shaved patients. Hair testing is most reliable for detecting prior frequent, heavy use of substances like cocaine, opioids, amphetamine, PCP, and Ecstasy, but not for detecting recent or occasional use.
Hair testing is well-suited for detecting chronic drug use, providing insight into a patient's long-term substance use pattern, and indicating periods of abstinence. Its main advantage is the longer window of detection compared to other matrices, limited only by the length of the hair sample and the degree of deposition in the hair. However, this long window period is also a disadvantage; hair testing is not useful in substance abuse treatment or monitoring opioid pain or other addictive medications when frequent testing is required.
Disadvantages of hair testing include high costs, longer analysis times, and complex laboratory procedures. No point-of-care tests (POCTs) are available for hair samples. Environmental contamination remains a concern, and controversies exist regarding the influence of biophysical attributes on hair analysis. Studies have shown that drug concentrations in hair can be affected by hair structure, growth rate, melanin content, hygiene, and cosmetic treatments. Hair testing may be biased towards some hair types, with drugs of abuse binding more readily to Africoid and Mongoloid hair compared to Caucasoid hair. Cosmetic hair treatments can also impact drug binding. In light of these factors, hair testing may not be the most equitable drug testing matrix.

Breath
Numerous user-friendly and precise breath-testing devices are available to detect recent alcohol consumption. While breath testing is primarily employed in alcohol treatment programs, it is not as common in primary care settings. Additionally, breath testing can be utilized to identify and quantify various other volatiles, particularly in industrial hygiene situations.
The body metabolizes alcohol rapidly, and alcohol remains detectable in breath as long as it is present in the bloodstream. The detection period for ethyl alcohol is merely hours, not days, after the last use. It is important to note that alcohol metabolism varies significantly based on an individual's gender, age, physical condition (particularly liver health), and weight.
Convenient breath alcohol tests can confirm alcohol ingestion within the past several hours. When administered properly, a breath alcohol analyzer test offers an accurate measurement of breath alcohol content (BrAC), which serves as an estimate of blood alcohol level (BAL). Factors such as body temperature and breathing patterns can influence breath alcohol test results.
Compared to blood and urine tests, breath tests are less accurate, with some evidence suggesting they may underestimate BALs by about 8.5%. Breath alcohol analyzers, like the well-known Breathalyzer, provide accurate BrAC measurements. These devices offer several benefits, including their simplicity, affordability, instant results, and noninvasive nature.
The National Highway Traffic Safety Administration maintains a list of breath alcohol analyzer devices that have been tested for accuracy and reliability, which is accessible at https://www.dot.gov/odapc.

Meconium
Meconium, the first few bowel movements of a neonate, serves as a useful tool in detecting neonatal exposure and maternal substance use during the third trimester of gestation. This unique matrix offers a broad window for drug detection, primarily focusing on drug use throughout the third trimester. Since the collection process is noninvasive, involving only the transfer of meconium from the diaper to a specimen container, it is typically more straightforward than urine collection. To ensure accurate results, it is essential to collect the specimen before the neonate passes their first formed stool, which usually occurs within three days for full-term babies.
Despite its benefits, meconium testing is a highly specialized area often used in conjunction with maternal urine drug tests. It is crucial to recognize the potential medicolegal ramifications of meconium testing, as a positive result may lead to the state removing the newborn from the mother's custody.
There are also some disadvantages to using meconium for drug detection. Test results can greatly vary based on substances used and cutoff concentrations due to meconium's unique properties. Additionally, laboratory methods for preparing the specimen can significantly impact the test results. Furthermore, urine contamination may skew the results.
The role of sampling swab drug tests in modern drug detection techniques is undeniably significant. These tests have emerged as convenient, noninvasive, and cost-effective tools for detecting drug use in various settings. Swab drug tests have been successfully integrated into law enforcement, workplace, and clinical environments, offering rapid results and helping to address substance abuse issues more effectively.
As technology continues to advance, it is expected that swab drug tests will become even more accurate and reliable, further solidifying their position in the field of drug detection. However, it is essential to remember that swab tests are just one part of a comprehensive drug detection strategy. Combining swab tests with other detection methods, such as urine, blood, or hair analysis, can provide a more complete and accurate picture of an individual's drug use history.
Ultimately, the key to effective drug detection and management lies in the ongoing collaboration between researchers, healthcare professionals, law enforcement, and policymakers. By working together and continuing to refine and expand drug detection techniques, society will be better equipped to address the complex and evolving challenges posed by substance abuse.

Source:
-
1. Embattled TV host Andrew O'Keefe charged with drug driving
References:
-
1. Bosker WM, Huestis MA. Oral fluid testing for drugs of abuse. Clin Chem. 2009 Nov;55(11):1910-31. doi: 10.1373/clinchem.2008.108670. Epub 2009 Sep 10. PMID: 19745062; PMCID: PMC3165054.
-
2. Musshoff F, Madea B. Review of biologic matrices (urine, blood, hair) as indicators of recent or ongoing cannabis use. Ther Drug Monit. 2006 Apr;28(2):155-63. doi: 10.1097/01.ftd.0000197091.07807.22. PMID: 16628124.
-
3. Boumba VA, Ziavrou KS, Vougiouklakis T. Hair as a biological indicator of drug use, drug abuse or chronic exposure to environmental toxicants. Int J Toxicol. 2006 May-Jun;25(3):143-63. doi: 10.1080/10915810600683028. PMID: 16717031.
-
4. Kacinko SL, Jones HE, Johnson RE, Choo RE, Huestis MA. Correlations of maternal buprenorphine dose, buprenorphine, and metabolite concentrations in meconium with neonatal outcomes. Clin Pharmacol Ther. 2008 Nov;84(5):604-12. doi: 10.1038/clpt.2008.156. Epub 2008 Aug 13. PMID: 18701886; PMCID: PMC2714885.
-
5. Gareri J, Klein J, Koren G. Drugs of abuse testing in meconium. Clin Chim Acta. 2006 Apr;366(1-2):101-11. doi: 10.1016/j.cca.2005.10.028. Epub 2006 Jan 17. PMID: 16413011.
-
6. Gray TR, LaGasse LL, Smith LM, Derauf C, Grant P, Shah R, Arria AM, Della Grotta SA, Strauss A, Haning WF, Lester BM, Huestis MA. Identification of prenatal amphetamines exposure by maternal interview and meconium toxicology in the Infant Development, Environment and Lifestyle (IDEAL) study. Ther Drug Monit. 2009 Dec;31(6):769-75. doi: 10.1097/FTD.0b013e3181bb438e. PMID: 19935364; PMCID: PMC2784609.