News and Blogs
Is HPV Self-sampling The Future of Cervical Cancer Screening?
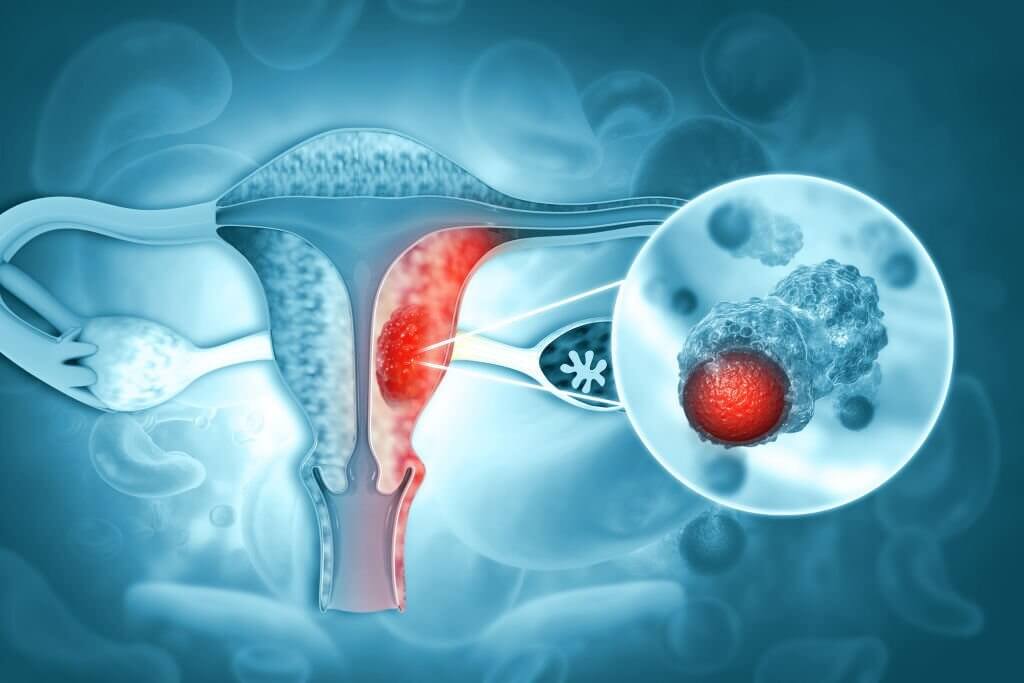
Self-sampling for human papillomavirus (HPV) testing is a method where individuals collect their own sample, typically from the vagina, that will then be tested for HPV. This is an alternative to having a healthcare professional collect the sample, which is usually done through a cervical swab during a pelvic exam (as part of a Pap test or HPV test).
There are two common types of self-sampling methods:
- 1. Vaginal swab: The individual is given a device similar to a cotton swab but with a longer handle. They insert the swab into their vagina, following the instructions provided, and then place it into a special container to be sent to the lab.
- 2. Urine sample: Some studies are looking at the possibility of detecting HPV in urine samples, though this method is not as common or established as the vaginal swab.
Self-sampling can be done in the privacy and comfort of one's own home, which can make it a preferable option for some individuals. It may be particularly beneficial in situations where access to healthcare providers is limited, such as in rural areas, or for individuals who may feel discomfort or anxiety about undergoing a pelvic exam.
Research has shown that self-sampling for HPV testing can be effective and reliable. Studies have found the accuracy of self-collected samples to be comparable to those collected by healthcare professionals, though it may vary depending on the exact methods and technologies used. Importantly, self-sampling has been found to increase participation rates in HPV screening programs, which can lead to earlier detection and treatment of precancerous conditions and reduce the incidence of cervical cancer.
However, it's important to note that while self-sampling can test for the presence of HPV, it cannot diagnose cervical cancer or other HPV-related diseases. If a self-sampled HPV test is positive, a follow-up visit to a healthcare provider is necessary for further testing and evaluation. The specific recommendations may vary depending on the guidelines in different regions or countries.
It's also crucial that individuals follow the instructions provided with the self-sampling kit to ensure the sample is collected properly. Improper sample collection could potentially lead to inaccurate results.
Self-sampling for HPV testing may increase the screening for and early detection of cervical cancer, which can potentially decrease its global burden. This testing method is seen as a significant opportunity to enhance cervical cancer screening uptake, particularly among under-screened women.
One study reported that self-sampling on filter paper had a sensitivity of 66.7% (meaning that it correctly identified 66.7% of true HPV cases), a specificity of 100% (meaning it correctly identified all non-HPV cases), a positive predictive value (PPV) of 100% (meaning all positive results were true positives), and a negative predictive value (NPV) of 59.1% (meaning it correctly identified 59.1% of true negative cases).
Do self-sampling kits actually increase screening participation?
Numerous studies have shown that mailing HPV self-sampling kits directly to patients’ homes dramatically increases participation in cervical cancer screening, especially among underscreened populations. Meta-analyses found on average a 2-3 fold higher response rate compared to mailing invitations for a Pap smear. For example, while only 7-10% of women responded to Pap smear reminders in some studies, 26-39% responded when offered a self-sampling kit. The convenience and privacy seem to spur more women to get screened.
Is HPV testing on self-samples as accurate as clinician-collected samples?
Extensive research indicates HPV testing on vaginal self-samples has comparable accuracy to physician-collected cervical samples. Meta-analyses show excellent agreement in HPV detection between the two methods, with similar sensitivity and specificity. PCR-based HPV assays perform particularly well on self-samples. Studies consistently find 90% or higher concordance in HPV results between self- and clinician-sampling. At-home screening can deliver the same high standards as the clinic.
Do women prefer self-sampling over clinician visits?
The majority of studies find women prefer vaginal self-sampling at home versus undergoing a pelvic exam by a doctor. Self-sampling is perceived as more comfortable, convenient, and less embarrassing.surveys indicate women appreciate the privacy and autonomy. Avoiding the clinic provides a major advantage over traditional Pap smears for many underscreened women.
Does a positive HPV result motivate follow-up?
A major concern is that women testing positive by self-sampling may not seek appropriate follow-up care. However, research shows 75-90% of HPV+ women went for clinician diagnostic testing after self-sampling in trials. The at-home screening seems to motivate underscreened individuals to address cervical health issues where they otherwise may not have. Self-sampling paired with clinical follow-up provides a promising comprehensive approach.
Are countries adopting self-sampling programs?
Given the accumulating evidence, several countries are now incorporating self-sampling into official cervical cancer screening recommendations. The Netherlands pioneered national HPV self-sampling programs. Australia, Finland, the UK, and others have followed suit. The U.S. is currently conducting trials to evaluate adding this option. The accessibility of home-based screening is making cervical cancer prevention more feasible and effective worldwide.
HPV self-sampling kits address major barriers to clinical screening participation while maintaining accuracy. This innovative screening strategy empowers more women to take control of their cervical health. More widespread adoption could reduce cervical cancer incidence and mortality, especially among high-risk, marginalized populations. At-home HPV testing provides a promising new direction for preventive care.
Click to View → Mantacc Cervical Specimen Collection Kits
References
- 1. Self-sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis
- 2. Offering HPV self-sampling kits: an updated meta-analysis of the effectiveness of strategies to increase participation in cervical cancer screening
- 3. Diagnostic study of human papillomavirus DNA detection in cervical and vaginal samples using the filter paper card
Related Posts
HPV Infection: Pathogenesis, Screening, and Prevention
The Ideal Swab for HPV Testing
HPV in Men: Key Findings From The HIM Study
At-Home HPV Testing: The Gift of Cervical Cancer Prevention






