News and Blogs
A complete guide to cervical swabs: key tips explained
Clinical operation guide and precautions for cervical swab
In the field of gynecological screening, cervical swabs are an important cell collection tool, and their standardized use directly affects the accuracy of detection. This article takes two cervical swabs, 95000LV and 95000L, produced by Mairekolin Medical Technology (ceded ISO13485 certification) as an example, and explains the operating procedures and taboos of different models in detail.
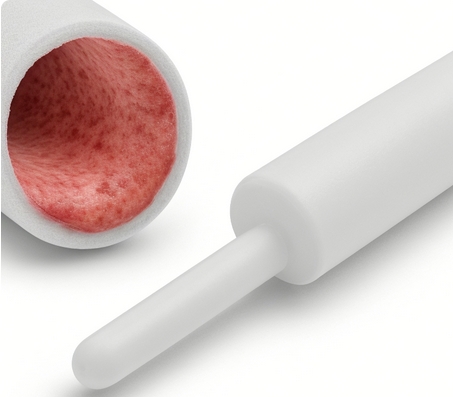
1. Standard operating procedures for 95000LV type cervical swab This model adopts an innovative spiral cannula design, and its medical-grade ABS material can ensure sterility in the sampling process. Pay attention to the operation: 1. The subject is kept semi-lying, and the operator holds the anti-slip handle and puts the cannula vertically into the vagina until the safety limit piece contacts the vaginal opening (at this time the foam brush head is inside the cannula) 2. Rotate the handle clockwise for 5–6 weeks so that the polyester fiber brush head fully extends out of the cannula and fully contacts the cervical squamous columnar epithelium junction area 3. When exiting the instrument at a constant speed, the sampling brush must be placed in a container containing 20ml of cell storage solution, and oscillates vertically for 12 times (recommended frequency 2 times/second) to release the cell sample 4. Seal the transport bottle immediately and send it to the test within 4 hours under 2-8℃ environment.
2. Key points of the 95000L double snap cervical swab operation. The unique double-position snap design of this model can accurately control the sampling depth. Clinical data shows that its cell capture rate is 98.6%: 1. In pre-installed state, the sampling brush disc should be located in the middle of the upper and lower snap buckles (8mm spacing), ensuring that the brush head is completely stored in the polypropylene cannula 2. The insertion depth is based on reaching the outer cervix (average insertion depth is 7-9cm), and the operating resistance should be controlled within the range of 0.5-1.2N. 3. After pushing the brush handle to completely expose the brush head, it needs to rotate 4–5 turns in a single direction (about 30 seconds). This operation can collect about 2×10⁴ epithelial cells. 4. When breaking the sampling rod, special grooves are required. The number of oscillations of the storage liquid directly affects the DNA release rate (study shows that the effect of 15 oscillations is the best)
3. Contraindications and risk prevention and control of cervical swabs. According to the 2023 gynecological diagnosis and treatment consensus, cervical sampling is prohibited in the following situations: • Those without a sexual life history (complete hymen) • Menstrual period (endometrial dissection affects detection accuracy) • Pregnancy period (operation may induce uterine contractions) • Lactation period (hormone levels interfere with cell morphology) In special circumstances, it is recommended to give priority to the use of vaginal ultrasound-guided cannula positioning technology, which can reduce the risk of tissue damage to 0.3mm. If there is a slight bleeding (<5ml) after the operation, a sterile cotton ball can be used to compress the bleeding.
Clinical practice shows that the pass rate of samples for correct use of cervical swabs can reach 97.8%, while operational errors may lead to false negative results up to 23%. It is recommended that medical institutions conduct NCCL standardized sampling technology assessments on operators every quarter to ensure the quality of cytology detection.
Contraindications and restrictions on use When there are abnormalities in the reproductive system, cervical sampling operation should be postponed.
Specific contraindications include: patients who have recently undergone cervical surgery (such as KEEP cone, cryotherapy or laser treatment), it is recommended to undergo cytology tests at least three months after surgery. Clinical data show that premature postoperative sampling may lead to false negative results of 15%-22%. Patients with acute cervicitis need to undergo anti-inflammatory treatment first, and samples will be taken after the C-reactive protein level returns to normal range.
Special precautions Before sampling, specific preparation specifications must be followed: It is recommended to perform operations on the 7th to 14th day of the menstrual cycle, when the cervical mucus viscosity is most suitable for sample collection. Sex and bathing should be strictly avoided 24 hours before operation to avoid damaging the cervical microenvironment. The American Academy of Obstetrics and Gynecology (ACOG) study pointed out that failure to comply with this specification may lead to more than 30% of sample contamination rates. For those with sensitive special materials, it is recommended to give priority to medical-grade polyester fiber flocking swabs, which have a three-dimensional structure that improves cell collection efficiency by 67% compared with traditional sponge materials.
Key points of standardized operation must confirm product integrity before use: independent packaging should have ISO13485 certification mark, and products with damaged packaging or exposed brush heads are at risk of microbial contamination. Clinical statistics show that the incidence of discomfort under standardized operations is less than 0.3%, but it should be noted that the sampling force should be controlled within the pressure range of 200-300g. After operation, the samples need to be transferred to a storage tube containing Preserved solution within 2 hours, which maintains cell activity for up to 6 weeks.
Material selection is recommended. Currently, mainstream cervical swabs are divided into two categories: biphasic flocking structure and sponge adsorption. The flocking material achieves rapid cell transfer through capillary action, which improves diagnostic sensitivity by 40% compared to traditional materials.